‘Documenting is something I have to do. I tolerate it so I can see patients.’
This was the fifth interview in the past month and each interviewee thought documentation sucked. The interviews exposed a weird, depressing energy with patient documentation. Talking to clinicians who did it by hand, I heard a bizarre nostalgia because while relatively worthless it was faster. Electronic medical record (EMR) users were more uniform in their complaints; the forms did not match the clinical experience and it seemed to increase documentation workload instead of decreasing. Most documented patient sessions during evenings and weekends.
The basic take away? No one liked their EMR and hated documenting.
Poorly constructed documentation is a burden and disrupts the provider and patient experience
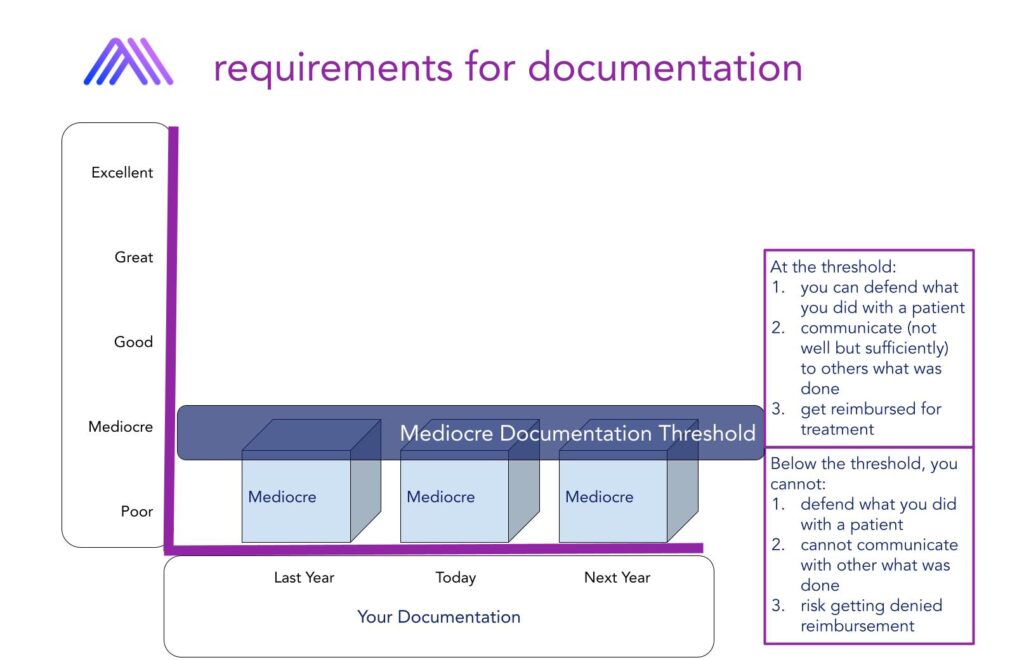
Documenting is required by law as a medical professional; doing it well is not.
Learning professional documentation in school revolved around two concepts; a defense against getting in trouble, defensible documentation, and communicating to a hypothetical colleague who may need to take over a patient’s care. Neither of these things push you to get better at documenting. It’s more a case of what is the least I can do while not getting in trouble.
As for my colleague, I could talk about the case and within seconds communicate more than what my documentation detailed. The third reason emerged when I got out of school and started practicing.
We needed certain information so the insurance company paid for care.
The three main reasons basically set the bar of documentation. The level was mediocre documentation.
No class existed on building a smooth experience or on what value great documentation brings to your clinical practice. Instead, you hear scare tactics about some physical therapist getting brought before the board with terrible records. If only they had better documentation, they would have been safe from the complaint.
But documentation can be incredibly valuable, change how you practice for the better, and most importantly, not suck to do.
Documentation is a skill
Documenting is a skill.
It takes work to get the right information down in the EMR and finish the note in a specific amount of time. One key aspect of the skill set is documentation in session. This means documenting while the patient is with you. Documenting in session is a critical aspect of the documentation skill, but most clinicians despise it.
Here is a snapshot of responses when asked about documenting in session:
- ‘It takes away from the patient experience.’
- ‘I feel it interrupts my workflow.’
- ‘I take notes on a piece of paper and then type it into the EMR later.’
- ‘There is too much information to put down so I just get most of it in later.’
The majority reported significant documentation outside of the session because documenting in session ruined conversation, data entry problems, and the use of other, more comfortable analog methods like writing in a notebook that required transferring the information in later.
With the electronic revolution, why does the act of using the technology during the session cause so many complaints?
Because documentation mastery requires a lot of work prior to the patient session.
The 6 reasons documentation is terrible for practitioners
There are six issues that make in session documentation terrible:
- You do not have clear and consistent clinical workflow
- You do not have a documentation workflow.
- You do not have a clear documentation structure that brings together the clinical and documentation workflow.
- There is no perceived value to the clinician outside of not getting trouble, limited communication to other team members, or getting reimbursed (this lack of perceived value transfers to the patient who thinks you are wasting their time).
- Too much free text; not enough time saving entry methods or information usable for feedback
- The work of today never makes tomorrow better (no documentation system)
Each of these issues can be improved. In many cases, you have a hidden process or two. They cannot remain hidden. You must bring them out and get clarity. We will help you do that. Let’s see how.
You do not have clear and consistent clinical workflow
The clinical workflow is the first step to documentation mastery. If you do not have a clear idea of how you move through a patient interaction, you cannot document it well. If you cannot document it well, there is no feedback for improvement. If you do not get feedback, you cannot improve. It all starts with knowing your clinical workflow.
You have no in session documentation workflow
The documentation workflow is not the clinical workflow. The documentation workflow is specifically how and when you put information down. You need to master session documentation strategies and know how to efficiently finish the document. This process is called your documentation workflow.
You do not have a clear documentation structure that brings together the clinical and documentation workflow
The clinical actions does not clearly synergize with how you document. This is clear by how many people hate documentation. Considerable work must be done at the underlying structure to bring out the best synergy and standardization. This includes ways to signal issues for improvement, naming conventions for forms, and standards for data entry. Further, documentation must improve the quality of the session experience. This is a perspective shift from seeing documentation as a burden to viewing it as a tool. The possibilities for documentation grow and improve when viewed as a tool to make work better. This is all structural.
There is no perceived value to the clinician outside of not getting trouble, limited communication to other team members, or getting reimbursed
Documentation can be incredibly valuable. It is the underlying driver of the big data revolution. Unfortunately that is hard to see when drowning with a busy schedule and a poorly constructed documentation system. The risk of getting in trouble because of crappy documentation is not motivating, however knowing that you can improve your own methods without needing to go to another continuing education class is incredibly motivating. Documentation mastery means you get help in session and outside of the session.
Too much free text; not enough time saving entry methods
If you are typing everything out is session, it is almost impossible to have documentation mastery. This the most common snag – too much free text- that we see in poorly constructed documents. You must move from the typical free text response into categorical variables, drop downs, multiple choice, and more.
The work of today never makes tomorrow better
You must have a documentation improvement cycle. Documentation mastery requires constant, consistent refinement. Your practice is not stagnant. It grows and morphs. The documentation must be responsive to this or you will be in this issue again a year from now.
Start now
Documentation mastery is possible but you need to start today.
We strongly recommend starting at the clinical workflow. Reformatting your forms seems like the best place to start, but we consistently find this to not help. It was confusing for a while until we realized that the jumping into documentation formatting did not help if you don’t understand your current process.
If you want help developing a clinical workflow, schedule a free documentation mastery consultation.

